Some of you may have heard that I was in the hospital
recently. Over the past few days, I have
finally had a chance to do some research into my current health situation in an attempt to better understand it myself. I am sharing my story with the hope that it can help inform others
who have not heard of these conditions.
If you have any
questions, suggestions or feedback,
please feel free
to leave a comment here or to get in touch with me!
◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇
It is a bit surreal to recall that, just last week, my life was a whirlwind of
hospital beds, doctors, nurses, specialists, daily bloodwork, neurological
examinations, imaging tests, procedures, and an ambulance ride.
Ultimately,
I was diagnosed with a rare condition called carotid artery dissection,
which puts me at high risk for having a stroke. In some cases, this
condition leads to partial blockage of blood flow through the carotid artery to
the brain. In my case, however, the internal carotid artery on my right
side is completely blocked. I might also have a vascular
disease called fibromuscular dysplasia (FMD), which might have
caused the carotid artery dissection. I’ll be getting further testing to
determine if arteries in other areas of my body are affected by FMD. I've
also heard that there is a genetic test I may be able to take, so for my
relatives reading this – I will keep you posted. I also need to see an
ophthalmologist to determine what damage might have occurred to my right eye.
I am
so unbelievably lucky that I did not have a stroke. The vascular surgeon
agreed with my mom that I had “dodged a bullet”. I had no bleeding in my
brain. I had no neurological deficits.
Apparently, my body was able to compensate for the blocked blood flow
from the carotid artery by developing new vascular pathways to keep enough
blood going to my brain. How amazing is that? The human body is
such a delicate, complicated, incredible network of moving parts that never
ceases to astound me.
Please watch this brief video about FMD (less
than 2 minutes):
Here is a good overview of carotid artery dissection:
Five days in the hospital felt
like so much longer. I am grateful to
have access to high quality medical care close by, here in Houston. I am so grateful for all of the people who
helped me out along the way. It is
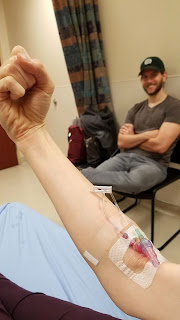
amazing how many different people one patient interacts with. I am grateful to no longer be tethered to all
the cords that made it challenging to sleep, get out of bed, and go to the
bathroom – heart rate monitor, blood pressure monitor, IV line, an oxygen
sensor taped onto my index finger, and compression devices attached to my lower legs
to prevent blood clots.
I was finally able to go home
one week ago, last Friday evening, where I’ve been instructed to get a lot of
rest and to “take it easy”. I have been prescribed blood thinners for long-term use, and pain medication and muscle relaxers for short-term use. The hope is that the blood thinners will help
my blood to flow better around the blockage and eventually begin to relieve the
pressure and pain on the right side of my head.
They will also reduce my risk of blood clots and stroke. I’ve been instructed to stop taking my
migraine prescription (Imitrex) and Advil, and to take Tylenol instead. Unfortunately, Tylenol doesn’t seem to work
very well for me. I am not sure how long
it will take to get back to “normal”. I
can’t read or write for extended periods of time without my eye and head
hurting, but I’m hopeful that I’ll be able to get back to my coursework and maybe
even finish off the spring semester on time.
The first few nights back home were a little rough, but I finally
started feeling some improvement a couple days ago, so I am becoming more
optimistic about my recovery process. I
am still experiencing some pain every day, but it has definitely gotten better. There is even a possibility that the
dissection will heal and the blockage will go away. I’ll be going back to the hospital for a
follow-up imaging test in 3 to 6 months to check on that.
Meanwhile, I’ve been catching up
on my favorite podcasts and charting out my new normal. One of my priorities is figuring out how to update my desk
setup so it is more ergonomic and minimizes strain on my neck, back and
eyes. I’m also trying to plan out a good
exercise program going forward. I want
to improve my vascular health – and if I can continue working on getting more
fit before my wedding in 7 months, that would be a fantastic bonus. However, I was told not to lift more than
10lbs or do ab work for the next 6 months because it can cause too much
strain. I can walk and jog, so I might
look into getting a treadmill or elliptical.
I was given the go-ahead to do cardio exercises, but nothing that causes
too much strain, particularly for my neck and head. Any recommendations?
If anyone wants to be a walking
buddy, let me know! There are some great
parks and neighborhoods around Houston and near me.
◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇
◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇For anyone interested in hearing a longer version of what my week in the hospital was like, here goes...
Monday 4/10
Last Monday morning, April 10th,
Seth took me to the emergency room at Cypress
Fairbanks Medical Center Hospital in northwest Houston with pretty bad head and
neck pain on my right side that had worsened over a few days. The peripheral vision of my right eye had
also been affected. My migraine medicine
– sumatriptan (Imitrex) – and some Advil had kept the situation manageable enough
from Wednesday through Saturday. Thinking
it was nothing more than a persistent headache, I was just trying to make it
through some schoolwork that was due Sunday and Monday for my online
classes. Since it was unusual for a
headache to last so long, I planned to go see a doctor on Tuesday. But by Sunday night, the pain kept me from
sleeping. The medicine wasn’t helping
anymore. Just laying my head on the
pillow made the pain worse. I felt
pressure in my ear and wondered if I possibly had an earache. It hurt to sneeze. My neck hurt so much whenever I swallowed. The right side of my face was sensitive to
even the lightest touch, especially around my temple, ear, and jaw joint. My neck was also sensitive to touch under the
jawline and at the right lymph node. I
knew this was definitely more than “just a migraine”.
Even so, I didn’t expect to be
admitted to the hospital overnight, much less for the entire week. At the ER, I first got bloodwork to check
whether my kidneys were healthy enough for me to get a CT scan. Apparently the contrast dye used in
diagnostic imaging such as CT scans can damage kidneys. The ER doctor, Dr. Hall, put numbing drops in
my eyes (those really stung) and used a device to measure my eye pressure. All looked good so far.
I was able to get the CT angiogram scan, which examined the
blood vessels and arteries in my head and neck.
When the contrast dye was injected into my IV line, it was a pretty odd
sensation. First a slightly metallic
taste arises in the back of your throat, then a warm sensation spreads through
your chest, trunk of your body, and limbs.
I was warned that it might feel like you’re peeing in your pants for a
minute! It sorta did!! The scan didn’t last too long, then I was
taken back to the private ER room to rest.
I think it was about an hour later when Dr. Hall came by to let us know
he had taken a preliminary look at the scans and luckily did not see any masses
or bleeding. That was welcome news. While we were waiting for the radiologist’s
official report, he said I could get a “migraine cocktail” – start with some
pain medication, add Benadryl, throw in a steroid, and top it off with an
anti-nausea med. I was definitely ready
for some pain relief. Before leaving the
room, he said, “Hopefully it’s just a migraine, and you can head home
soon.”
I asked the nurse, Brad, what a
person could do for some food around here.
He told Seth where the cafeteria was, but said I couldn’t eat anything
yet since they were not yet sure of my diagnosis. Oh well, at least I had my cocktail
coming. We joked with Brad that he must
have learned bartending as part of his medical training. Each part of the “cocktail” was administered
directly into my IV line, just like the iodine dye had been. One of the meds made my entire backside feel
tingly, like I was laying on a thousand tiny needles. I kind of jumped up at first, saying “It
feels prickly!” Brad gave me a quizzical
look and said, “Prickly...?” Then, when
the Benadryl was administered, I suddenly got really cold and it made my teeth chatter
like crazy. I felt like one of those
wind-up toys of the chomping set of teeth.
So, that was strange, but also funny as I lay there loudly chattering
away for a while. Thankfully a nurse came
back with a big, magical blanket, nice and warm like it was fresh out of the
dryer, and draped it over me – oh man, that was the best moment ever. The warmth of the blanket and drowsiness from
the Benadryl lulled me to sleep for a little while.
I’m not sure how much time
passed before I was abruptly awakened by Dr. Hall talking to me. He told me that according to the CT scan it
looks like I have something called a carotid artery dissection; that they would
be admitting me into the hospital and I would be there overnight. All I remember saying was, “Huh? Overnight?”
I was still waking up and trying to figure out what the heck was going
on. That was certainly the moment we realized
that $#!+ just got real.
 |
| MRI image. Now I know what I'd look like without hair. |
 |
| Dinner: meatloaf, mashed potatoes, and squishy flavorless vegetables. |
 |
| Room with a view. Nice after being in the window-less dungeon of the ER all day. |
 |
| Seth's accommodations |
 |
| OOTD! Rockin' my new duds and feeling good after my migraine cocktail |
Tuesday 4/11
 |
| EEG Medusa |
My dad, my brother Gabriel, and
his girlfriend Sydney came over that afternoon to provide entertainment, great
company, and bring Thai food for dinner.
Every time someone entered the small room, I loved the look of surprise
on their face upon realizing that 6 people were already crammed in there. When the neurologist came by to examine me,
the party had to move out into the hall for a bit. As my dad later said, “there was so much
silliness and hilarity that we decided to give her a break the rest of the week
so she could rest.” Thank you, Gabriel
and Sydney, for spending your last day in Houston together hanging out with
little ol’ me!
 |
| Aptly named game: Escape the Room |
 |
 |
Wednesday 4/12
Wednesday morning, we finally
got to meet with the vascular surgeon, who recommended that I be transferred to
another hospital for an angiogram. He
was the first person to mention the possibility of FMD being involved. I got another MRI – this time it was an MRA of my neck. After lunch I finally took a shower, which
was so nice just to be able to be out of bed for a while after two days of
being confined to beds and wheelchairs. We
packed up, and once all the transfer paperwork was complete, I was transferred
via ambulance to the Neuroscience ICU at St. Luke’s Hospital
in the Medical Center. Mom rode in the
ambulance with me, while Seth went home to prepare for staying at the new hospital
with me for a few days. Honestly, the
ambulance ride was a nice distraction for a little while. When they wheeled me outside on the
stretcher, before loading me into the back of the ambulance, it felt SO good
just to be outside and feel the sunshine again.
It was nice to watch the world outside of the ambulance windows,
too.
By the time I got settled into
the new room, it was around 8pm, and I was told not to eat or drink after
midnight in case I was getting the angiogram the next day. The hospital cafeteria was already closed, but
thankfully I was able to request dinner from the Lamanuzzi Kitchen, which Seth
delivered upon his arrival.
After
the procedure, I had to lay flat for 6 hours and not bend my right leg at
all. But – I could finally eat!! Seth fed me applesauce and chocolate pudding,
and it was glorious.
I even got a couple visitors that evening! My best friend Rebecca stopped by after work, and Seth’s cousin Elly came by a couple hours later.
A couple last notes, before
signing off. In trying to determine if
my dissection might have arisen in response to some type of trauma, I was asked many times if I had recently been to a chiropractor, gotten a massage, done
yoga or anything else that could have manipulated my neck in some way to cause
strain or injury. I was pretty surprised
that things like this could possibly lead to a tear in one’s artery. Although my dissection seems to have been spontaneous (rather than attributed to trauma), this is just a reminder to be aware of
what you’re doing to your body, and be gentle with yourself! And perhaps, think twice before getting your
neck “adjusted” at the chiropractor… make sure it is a gentle method.
Finally, I want to acknowledge
all of the caretakers in the world. I was
truly able to witness the village of humanity at work in my life. To know that similar networks are at work in
communities all throughout the globe brings me much joy and gratitude. From my wonderful friends and family, to the
gracious EMTs with the ambulance service from Patriot EMS, to all of the staff
from both hospitals – nurses, doctors, specialists, cleaning crews, kitchen
staff, administrative personnel, volunteers, medical students, residents, and
fellows – thank you! I enjoyed your
company, appreciate your kindness, and thank you for your efforts to keep the
world going ‘round. I didn’t need a
health scare to realize this, but it never hurts to be reminded – I know that I
am very lucky, and very loved. I will strive
to spend my time helping others feel the same, and I will continue to seek out
my own role in keeping this world of ours spinning.
.
If we had to be stranded in the
hospital for a while, we were definitely grateful that it was just down the
street from our favorite local restaurant, Mario’s Taco & Burger House – just what
the doctor ordered! Seth made a breakfast
taco run Wednesday morning, and I had to laugh when he handed me my potato
taco. Medicinal, indeed.
 |
| Can you spy what's missing on this MRA? Hint: my right side is shown on the left of the image. |
 |
| Farewell, Room 330 |
 |
| My first (and hopefully last) ambulance ride |
 |
| Mom 💚💗💜 |
 |
| Sandwich, fruit & cheetos, made fresh from the Lamanuzzi Kitchen with love and silliness. |
 |
| Just some light bedtime reading |
 |
| Hospital guest bed #2 |
Thursday 4/13
Thursday
morning brought a new round of doctors to re-tell my story and symptoms to, and
to continue the neurological exams. It
had become a kind of game for me, like an ice-breaker game for every new doctor
or medical student who came to see me. Each
person had a slightly different technique for doing the exam.
“Cover one eye. How many fingers am I holding up? Now how many?”
*brushes fingers along both
sides of my face* “Does this feel the same on both sides?”
*snaps near left ear* “Can you
hear this?” *now right ear* “How about
this?”
“Hold both of your arms out,
palms up. Now push against me, don’t let
me bend your arm. Don’t let me bend your leg.
Don’t let me move your foot. Now
pull against me, don’t let me straighten your arms.”
“Clench your jaw.”
“Say ahh.”
*while moving their finger
around in the air* “Touch my finger, then your nose, now my finger again, and
your nose again.”
Etc., etc. They also hammered all over my arms and legs
to test my reflexes.
 |
| View from Room 7S4-7 |
All of a sudden they were ready to take me away for the
angiogram at 7am. We requested to speak
with the vascular surgeon or neurology fellow, and were able to have a nice
conversation with both of them to get a better understanding of the procedure and to ask some questions. Unfortunately, that
meant we missed our time slot and I couldn’t eat or drink for 6 more hours
until they could fit me in for the procedure later in the day. Luckily I was doing better this morning due
to another “migraine cocktail” I’d been given the night before, so I was
finally feeling well enough to make a few phone calls to friends and
family. Having been on the other side of
a loved one’s hospitalization before, I know how relieving it can be to
actually hear that person’s voice, and it was healing for me as the patient as
well.
At
1:30pm, the nurses wheeled my entire gigantic hospital bed out of the room and
through the halls, turning on the self-driving
mode of the bed – who knew?? That
was fun. Before I went in for the angiogram,
two of the medical personnel couldn’t agree where my pulse was in my feet and I
ended up with black and red permanent marker X’s decorating my feet. Also fun.
The procedure took about an hour and a half, I think. Check out these cool images they got:
 |
In the image on the right, the dissection is seen in the lower-right, just above the
spot where the main artery branches into the internal & external segments.
|
During the angiogram, considered an invasive procedure, a catheter was inserted near my groin and snaked all the way up to my carotid artery. Dye was injected, then x-rays taken to get a good look at the blood vessels. I was conscious throughout, but didn’t feel a thing. They needed me to be able to hold my breath a few times, I assume while they took some of the x-rays. This is when the doctors were able to determine that my internal carotid artery on the right side was fully occluded. When talking with the vascular surgeon after the procedure, we were all pretty shocked by that news. However, they were also able to see that I was getting enough blood flow through other vessels that had developed in order to keep all the necessary pathways connected. Apparently a more conservative approach – just taking blood thinners – was recommended as my best option for now, and is much less risky than any further procedures like angioplasty or placing a stent in the artery.
 |
| BEST PUDDING EVER after 17 hours of no food |
I even got a couple visitors that evening! My best friend Rebecca stopped by after work, and Seth’s cousin Elly came by a couple hours later.
I was counting down the minutes
til 9:40pm, written in large black marker on the board in my room to note the
time I could finally get up and move around again. I was determined to avoid using a bed pan if
at all possible, and happy to say that I made it – but I did buzz the nurse in
at 9:39pm to start disconnecting me from everything! What can I say – it was nice to have a goal to
work toward. Being in a hospital, the
focus of daily life tends to narrow to a few key areas: pain, sleep, food, and
bathroom breaks.
Friday 4/14
When
the nurse came in sometime around 3-5am to take my vitals and some bloodwork, I
got nauseous as soon as he lifted my bed into an upright position, and I was
sick for a little while. We guessed it
must have been due to the anesthesia from the procedure. Luckily he put some anti-nausea med into my
IV and I was okay after that. The doctor
came by early Friday morning to review some of the angiogram images with us,
and pointed out a couple spots of possible irregularities that might be FMD,
but it was not conclusive. The vascular
surgeon stopped by, too. We were informed
that the next step from here, in the short term, was just pain management. Since I had been at highest risk for having a
stroke when I first experienced the dissection, they felt I had been under
observation long enough that my risk had decreased enough to move out of ICU
into a regular hospital room. When I
heard mention of the possibility of being discharged, I perked up at that and
knew I would be more comfortable resting and managing my pain at home. The option to be discharged came as a
surprise to me, as I didn’t think I’d be able to bust outta there just yet. But by 1:30pm, we were in the car heading
home!
 |
| Thank you Nancy, John, Phil & Amanda It worked! |
 |
| Handmade gift from a hospital volunteer |
More Information:
1.
Carotid Artery Dissection
2.
Fibromuscular Dysplasia (FMD)
d. From
the journal Circulation: Fibromuscular Dysplasia: State of the Science and Critical Unanswered Questions -- A Scientific
Statement From the American Heart Association
.






No comments:
Post a Comment