Hello, friends. I've been meaning to revisit this space for quite some time. The last time I wrote in here, I had been recovering at home for about a week after being in the ICU and learning about some scary health issues. I intended to keep you updated and continue to document my journey. Well... the day after I made that blog post, I had a stroke. It was the morning of April 23, 2017. One year ago today.
It was the most terrifying moment of my life. I was so scared. Seth had never seen me so upset before. The ER doctor said that my symptoms of vertigo and nausea could "just" be from having a panic attack, but I knew it was a stroke first, which subsequently triggered the panic. I knew that being so upset probably wasn't helping, but I couldn't calm down. I tried to breathe.
I made it through. Another ambulance ride, another few days in the neuro-ICU. There is a lot to tell.
The truth is, it has been difficult for me to think about. It was such a traumatic experience that, whenever I go back to that morning, I feel all of the emotions all over again. It's a little better now, and with time I hope it has less of a hold on me. I needed time to process. I distracted myself from the health roller coaster by focusing on my upcoming wedding. The joy, togetherness, and gratitude I experienced surrounding my wedding were all very healing for me. Then it was the busy holiday season, and now another busy semester back at school.
One of the assignments in my English class this semester was to write a short memoir. I took that opportunity to finally return to this moment in my life that I had been keeping some distance from. I'll share my writing here, followed by some photos.
This repeats a few things from my previous post, but won't be as thoroughly documented. I have not yet gone back to ask for copies of the MRIs to share more neat images of my arteries. It's not a completely thorough account of my second time in the hospital, but, I am ready to put something out there. So here goes.
◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇
Dissection and Determination
Dissection and Determination
Rushing to the car, we made the
seven-minute-drive once again to the closest emergency room before dawn. The
last time my fiancé and I took this route almost two weeks prior, we were calm
compared to how we felt now. This time, I was extremely alarmed and could not
stop sobbing. Armed with the knowledge of my recent diagnosis, I knew I was
having a stroke, and I was utterly terrified that I might drop dead any second.
I had never felt so disconnected from my own body, knowing that I had
absolutely no control over what was occurring. The intensity and weight of this
realization was overwhelming and shattering. This was not supposed to be
happening! I had finally started feeling better since coming home from the
hospital. I had been taking the medications, sorting through all of the new
information, making follow-up doctor appointments, and preparing for my “new
normal”. As my reality was thrown into another tailspin, I had to figure out
how to navigate my way through to the other side.
The last time I went to the ER, I was
admitted to the intensive care unit for a couple days before being transferred
by ambulance to the neuro-ICU at a larger hospital. I was in a lot of pain, and
after many tests, imaging scans, and an invasive procedure, I was diagnosed
with a rare condition called carotid artery dissection. A tear in the inner
lining of this major artery on the right side of my neck caused a clot to build
up until it completely blocked off all blood flow from the internal carotid
artery to my brain. I was told at that time that I was unbelievably lucky that
I did not have a stroke. I had no bleeding in my brain and no neurological
deficits. Imaging showed that my body was able to compensate for the occluded
artery by developing new vascular pathways to keep enough blood going to my
brain. Rather than undergoing invasive procedures such as angioplasty or
placing a stent in the artery to open it up, a more conservative approach was
recommended. The hope was that the blood-thinning effects of a daily aspirin
would help achieve blood flow around the blockage and eventually relieve the
pressure and pain on the right side of my head. Feeling extremely lucky and
slightly optimistic, I was finally discharged and able to return home after
what felt like the longest five days ever.
However, my time of recuperation at home
did not last very long. Eight-and-a-half days later, I was bawling in the
waiting room of the ER, surrendering to the circumstance at hand and hoping the
nurses and doctors could fix me. It was 4:30am on a Sunday morning, one week
after Easter. At home, I had begun feeling dizzy, which was exacerbated and
accompanied by nausea whenever I tried to lay down. Upon feeling tingling and
weakness in my left arm and leg, I realized what was happening and tried not to
panic. At the hospital, I was unable to lay down on the hospital bed or CT
scanner without vomiting. After knocking me out with some medications, they
were finally able to get the necessary scans of my head and neck. The imaging
showed new vascular irregularities, so I was transferred via ambulance once again
to the neuro-ICU at the larger hospital, where further imaging determined
evidence of a small stroke. I also had new dissections, this time in my
vertebral arteries along the back of my neck. I learned to give myself
injections in my stomach so I could take the stronger blood thinner medication.
My doctor at the hospital told me to expect to be on it long-term, possibly for
my whole life. I was advised of serious risks such as internal bleeding,
cautioned not to travel to remote places in case of injury, and informed that I
could not have a viable pregnancy while on the medication. I was told that I
might have a vascular disease or a genetic abnormality that compromises the
structure of blood vessels, making them weaker and susceptible to damage, which
could be the cause of the dissections. It was difficult to process all of this,
and though I maintained my immense gratitude for how lucky I had been, I went
home feeling less optimistic this time. For a while, I kept a bag packed with
essentials and snacks just in case of another trip to the ER. My medical alert
ID bracelet arrived in the mail and became a daily reminder of my new reality.
My journey to recovery and good health
continues to be a roller coaster ride. A couple months after my last
hospitalization, I experienced a skin issue of itching and red hives all over
my body and face which became so severe that I ended up back in the ER. A skin
biopsy found that it was not an allergic reaction, but rather a rare subtype of
an already rare disorder called mastocytosis. I have to get regular lab work to
make sure it does not progress to leukemia or some other blood disorder.
Thankfully, I have been able to manage it pretty well on most days. Regarding
the dissections in my major arteries, I do have some genetic issues that can
“disrupt the integrity of my vascular system”, according to the doctor. I am
awaiting further genetic testing to acquire more information. I have had to
make big changes in my diet and lifestyle in order to manage my health
conditions and medications. Whenever I get a headache or feel some pain in my
neck, a familiar anxiety is triggered. I am still learning how to achieve
balance in my life, how to get enough rest and not overdo it. I may feel
perfectly fine for several days, and then I will experience some days of
extreme fatigue. The unpredictability is frustrating. However, there has been
some good news along the way, too. The peripheral vision in my right eye was
restored when the pressure from the blockage was relieved. I underwent
full-body imaging scans that ruled out a suspected vascular disease called
fibromuscular dysplasia. Additionally, the six-month follow-up scans of my head
and neck showed that, amazingly, the initial blockage in my carotid artery that
started all of this had fully healed! I could not believe it. My neurologist
said I could now just take baby aspirin every day instead of the stronger blood
thinners. I would no longer have to get my blood drawn every week to monitor
whether it was too thick or too thin. I was so happy to tell my family the
great news, and tears still come to my eyes whenever I think about it.
While facing my health issues has been
scary and painful, it has also been an adventure that continues to show me the
power of gratitude, self-care, support, and working together. It is quite
surreal to recall the whirlwind of hospital beds, doctors, nurses, specialists,
ambulance rides, daily bloodwork, neurological examinations, imaging tests, and
procedures. I am grateful to no longer be confined to bedrest and tethered to
all the cords that made it challenging to sleep, move around, shower, and go to
the bathroom—heart rate monitor, blood pressure monitor, IV line, oxygen sensor,
and compression devices to prevent blood clots. I am grateful for the ability
to go outside and feel the wind and sunshine whenever I want, instead of only when
being wheeled out on a gurney to take an ambulance from one hospital to
another. I am grateful to have access to high quality medical care, and I am so
grateful for all of the people who have helped me out along the way. I have
interacted with neurologists, vascular surgeons, anesthesiologists, medical
imaging technicians, EMTs with the ambulance services, hematologists,
phlebotomists, receptionists, and hospital staff including cleaning crews,
kitchen staff, administrative personnel, volunteers, medical students,
residents, and fellows. In the medical realm as well as in my personal life and
school environment, I was truly able to witness the village of humanity at
work. Knowing that there is a social structure in place to support and guide
each other through challenges that may arise in any of our lives has helped me
to make peace with the fact that there will always be elements outside of my
control. Like the human body, our society and communities are such delicate,
complicated, incredible networks of moving parts that never cease to astound
me. I am now able to embrace the unknown and move forward, day by day.
◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇◆◇
I was lucky. I had only a small stroke called a TIA (transient ischemic attack) that did not cause any lasting neurological damage. And YOU GUYS -- as many of you already know -- a little over 6 months after the stroke, I made it to my wedding!!! Without ending up in the hospital or covered in red blotchy hives!! It was amazing. My gratitude never ceases. 🙏
Onward.
~ Mia ~

 |
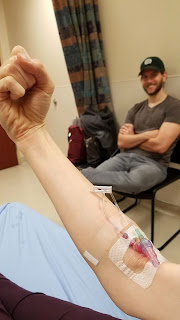
| (It's just a sensor that monitors my blood oxygen levels) |
 |
| Company / Entertainment |



 |
| After moving out of the ICU, this was my view of the Medical Center at night. |
 |
| If I was going to have to wear a medical ID for the rest of my life, I figured I might as well get a pretty one. |
 |
| Band-aid upgrade from Mom |

 |
| 6/23/2017: Back in the ER. This was after the IV steroids helped my hives subside. |
 |
| Hospital follow-up: full body MRI with contrast. |
 |
| 6-month MRI scans of head & neck. Y'all, I've had enough of the hospital gowns. |
 |
| Cool ceiling in the MRI room |
Different color every week.
|

 |
| 6/07/2017: Went to a presentation by my vascular surgeon, Dr. Jeremiah Johnson. |
 |
| When taking Coumadin (warfarin), Vitamin K interferes with the effectiveness of the drug to thin the blood. I really missed having salads! |

Coming soon.... wedding post! 👰🤵💗